To assess the prevalence of panic disorder during the second and third waves of the COVID-19 pandemic.
DesignCross-sectional multicenter study.
SettingPrimary care.
ParticipantsParticipating primary care physicians selected patients visiting their primary care centers for any reason over a 16-month period.
Main outcome measureDiagnosis of panic disorder was established using The Primary Care Evaluation of Mental Disorders (PRIME-MD) instrument.
ResultsOf a total of 678 patients who met the inclusion criteria, 36 presented with panic disorder, with a prevalence of 5.3% (95% confidence interval 3.6–7.0). A total of 63.9% of cases occurred in women. The mean age was 46.7±17.1 years. Socioeconomic difficulties, such as very low monthly income rate, unemployment, and financial constraints to make housing payments and to make ends meet were more frequent in patients with panic disorders as compared to patients without panic disorder. A high level of stress (Holmes–Rahe scale>300), concomitant chronic fatigue syndrome and irritable bowel disease, and having financial difficulties in the past 6 months were associated with factors of panic disorder.
DiscussionThis study characterizes patients with panic disorder diagnosed with a validated instrument during the COVID-19 pandemic and identified risk factors for this disease.
ConclusionsIn non-selected consecutive primary care attendees in real-world conditions during the COVID-19 pandemic, the prevalence of panic disorder was 5.3%, being more frequent in women. There is a need to enhance primary care resources for mental health care during the duration of the pandemic and beyond.
Evaluar la prevalencia del trastorno de pánico durante la segunda y tercera olas de la pandemia por COVID-19.
DiseñoEstudio transversal multicéntrico.
EmplazamientoAtención primaria.
ParticipantesLos médicos participantes seleccionaron a pacientes atendidos en atención primaria por cualquier motivo durante 16 meses.
Medición principalTrastorno de pánico diagnosticado usando el cuestionario Primary Care Evaluation Mental Disorders (PRIME-MD).
ResultadosDe un total de 678 pacientes elegibles, 36 presentaban un trastorno de pánico, con una prevalencia del 5,3% (intervalo de confianza del 95% 3,6-7,0). Un 63,9% de los casos se presentaron en mujeres. La edad media fue de 46,7±17,1 años. Las dificultades socioeconómicas, como bajos ingresos mensuales, falta de empleo y restricciones económicas para pagos de la vivienda y llegar a final de mes eran más frecuentes en los pacientes con trastorno de pánico que en aquellos sin. Los factores asociados al trastorno de pánico fueron un alto nivel de estrés (escala de Holmes-Rahe > 300), síndrome de fatiga crónica concomitante e intestino irritable y dificultades económicas en los últimos 6 meses.
DiscusiónEste estudio caracteriza a los pacientes con trastorno de pánico diagnosticados mediante un instrumento validado durante la pandemia por COVID-19 e identifica los factores de riesgo.
ConclusionesEn pacientes consecutivos no seleccionado en condiciones del mundo real durante la pandemia por COVID-19, la prevalencia del trastorno de pánico fue del 5,3%, siendo más frecuente en mujeres. Es necesario aumentar los recursos para la salud mental durante y más allá de la duración de la pandemia.
The coronavirus disease 2019 (COVID-2019) has been a major threat to public health worldwide, with associated multi-dimensional adverse effects on physical, mental, social, and emotional well-being. The mental health consequences of COVID-19, such as psychological distress, fear, stress, anxiety, and depression have been related to several factors, including quarantine and lockdown, loneliness, social distancing, perceived risk of contracting SARS-CoV-2 infection, and concerns about employment, finances, and personal safety or safety of family members.1–6 A study of the impact of the COVID-19 pandemic at first year in a representative sample of the adult Spanish population showed a statistically significant loss of weight, less use of tobacco and decreased disability for physical health, whereas there was a significant increase of major depressive episode and prevalence of general anxiety disorder for mental health.6 However, individuals who declared they had been diagnosed with COVID-19 showed a worsening in physical health and an increase in mental health problems and post-traumatic stress disorder symptoms.6
Primary care physicians are frequently the first point of contact of subjects with mental health problems, and the manifestations of mental disorders and associated comorbidity have become major issues in primary care.7–9 It has been extensively recognized that the consequences of significant declines in economic activity may constitute important stressing factors with a negative impact on mental health.10,11 In an analysis of the World Health Organization (WHO) of the impact of economic crisis on mental health in the European Region, an integrated response across policy actions that must include accessible health services, with a focus on primary care response has been explicitly recommended.12 However, there is limited data available on the effect of economic crisis with a rise in unemployment, depressed housing markets, severe cuts on public spending, and threats of recession from the perspective of the burden of mental health disorders attended by primary care physicians in the real-world setting.
The economic crisis that began in 2007 affected nearly all European countries, but the effects have been among the worst in Spain. Two studies, one in the pre-crisis period of 200613 and another in 2010–201114 investigated the frequency of mood, anxiety, somatoform, alcohol-related, and eating disorders in randomized samples of patients attending primary care centers and using the Primary Care Evaluation of Mental Disorders (PRIME-MD) instrument for the diagnosis of mental disorders. The 2010 survey showed a substantial increase in the percentage of patients with major depression, anxiety, somatoform disorders, and alcohol-related disorders, with household unemployment and mortgage payment difficulties as combined risk factors for mental health disorders.14 On the other hand, after the COVID-19 pandemic begins to recede, the subsequent economic crisis will have a knock-on effect on the mental health of the general population, with a direct effect on increasing attendance of mental health-related consultations in primary care.15 In addition, economic and healthcare sectors raise their uncertainties about the impact of this new crisis, due to its specific characteristics (e.g., globalization, incidence in highly sensitive sectors in Spain such as tourism, sequelae of the pandemic, fear of the resumption of activities, unsolved mourning the death of loved ones, etc.) that could reproduce or worsen the situation of 2009–2010.15
The aim of the study is to assess the impact of the COVID-19 crisis on the prevalence of panic disorders in primary care.
Materials and methodsStudy design and patientsBetween December 1, 2020, and March 25, 2022, an epidemiological, cross-sectional, and multicenter study was conducted in patients attending primary care consultations throughout Spain in daily practice conditions. The primary objective of the study was to assess the prevalence of panic disorder in the patient population attended in primary care in the current economic situation of the COVID-19 pandemic. The secondary objectives were to assess the sociodemographic and socioeconomic profile as well as the clinical characteristics of these patients, as well as the number of external stressors. Inclusion criteria were patients 18 years of age or older attending primary care visits for any medical complaint, with cognitive ability to understand and answer the study questionnaire and providing the written informed consent. Exclusion criteria were language limitations or the presence of any medical or psychological condition that involved the inability or unwillingness to follow the study procedures.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Clinical Research Ethics Committee (CEIC) of Hospital Clínico San Carlos (code 20/701E, 2020). Written informed consent was obtained from all participants.
The study included a single face-to-face interview in which the study questionnaire was administered and completed by the primary care physician. Participating physicians were selected through e-mail invitations sent to the members of the Spanish Society of Primary Care Physicians (Sociedad Española de Médicos de Atención Primaria, SEMERGEN), and the Spanish Society of General and Family Physicians (Sociedad Española de Médicos Generales y de Familia, SEMG), as well as to primary care physicians included in Medynet database (www.medynet.com), which is the first Internet node exclusively devoted to the healthcare sector in Spain that currently includes data of approximately 190,000 users. The study questionnaire was lodged in an Internet microsite that could be accessed via a weblink included in the e-mail. Only primary care physicians who accepted to participate in the study were provided with the microsite URL and the user's password.
Patients were administered a validated Spanish version of the PRIME-MD,16 which assesses different groups of mental diseases commonly diagnosed in the primary care setting, which included depressive disorders, anxiety disorders, somatoform disorders, and alcohol and eating-related disorders based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnostic criteria. It consists of two principal components: a patient's questionnaire completed by the patient and a structured interview (Clinical Evaluation Guide) completed by physicians. Both components were used. Primary care physicians were properly trained and familiarized with the PRIME-MD as they have been participated in previous similar studies in which this instrument was used.13 The mean time to complete the questionnaire is about 10min, and the psychometric values of the PRIME-MD for the diagnosis mental diseases included a sensitivity of 81.4%, specificity of 66.1%, negative predictive value of 83.4%, and positive predictive value of 62.9%.17
For each patient the following data were recorded: sociodemographic and socioeconomic characteristics, concomitant diseases, and the amount of stress using the Holmes and Rahe Stress Scale.18 This scale has 43 items and each item is assigned a certain number of points based on its perceived stressfulness, with statements to answer “yes” or “no”. Overall, total scores can range from 0 to 430. A score>300 indicates high stress, a score between 150 and 300 a moderate amount of stress, and a score<150 (0–149) a low level of stress. The study questionnaire is described in the Supplementary Material (Table S1).
Statistical analysisThe sample size was estimated assuming a confidence level of 95%, a type 1 error of 3%, and an expected proportion of mental health problems in our population of 15.7% based on previous studies.13,14 A total of 565 patients were needed, which increased approximately up to 707 patients for a percentage of losses of 20%. To achieve this sample size of 707 patients, a maximum number of participating physicians was established. It was expected that a total of 400 primary care physicians distributed throughout the Spanish autonomous communities could participate in the study, with 5 consecutive patients recruited by each of them. Categorical variables are expressed as frequencies and percentages with 95% confidence intervals (CI), and continuous variables as mean and standard deviation (± SD). The distribution of variables in the groups of patients with and without panic disorder was compared with the Fisher's exact probability test and the Student's t test for qualitative and quantitative data, respectively. Variables with a p value<0.2 in the bivariate analysis were included in a stepwise logistic regression model to assess independent variables associated with panic disorder. The Hosmer–Lemeshow test indicated a good fit of the model (Chi square=1.485, degrees of freedom=2, p=0.476). Regarding the presence of heteroscedasticity, the expected participation of 400 primary care physicians distributed throughout the national territory was planned, who in total registered 678 patients, so it was not considered necessary to adjust the model for the origin of the consultation. Statistical significance was set at p<0.05. The Statistical Analysis Systems (SAS) (SAS Institute, Cary, NC, USA) version 9.1.3 Service Pack 3 was used for the analysis of data.
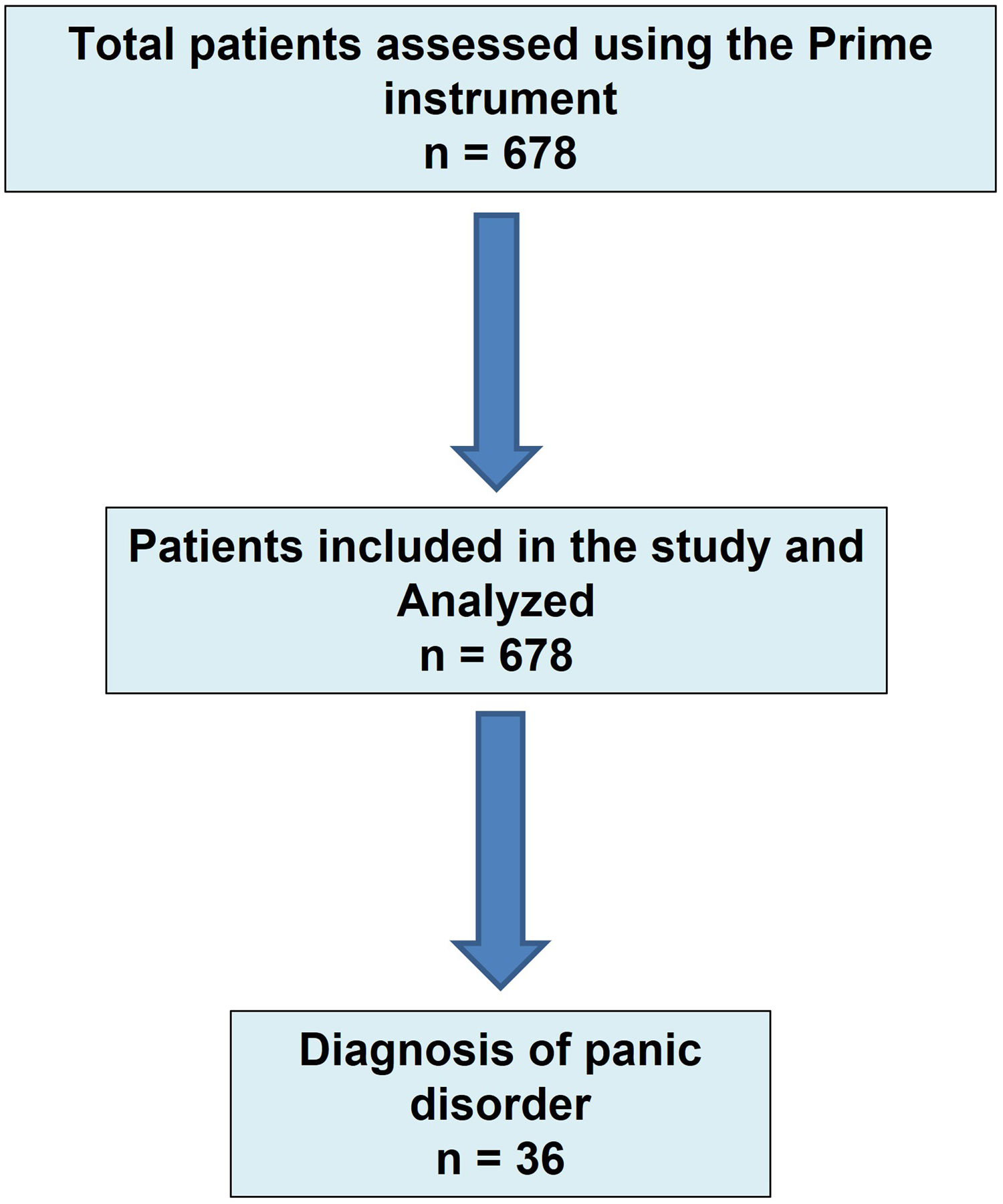
ResultsDuring the study period, a total of 678 patients met the inclusion criteria for which complete data of the study questionnaires were recorded. These patients were recruited by a total of 111 primary care physicians. Thirty-six patients were diagnosed with panic disorder (Fig. 1), with a prevalence of 5.3% (95% CI 3.6–7.0). There were 13 men and 23 women, with a mean age of 46.7±17.1 years.
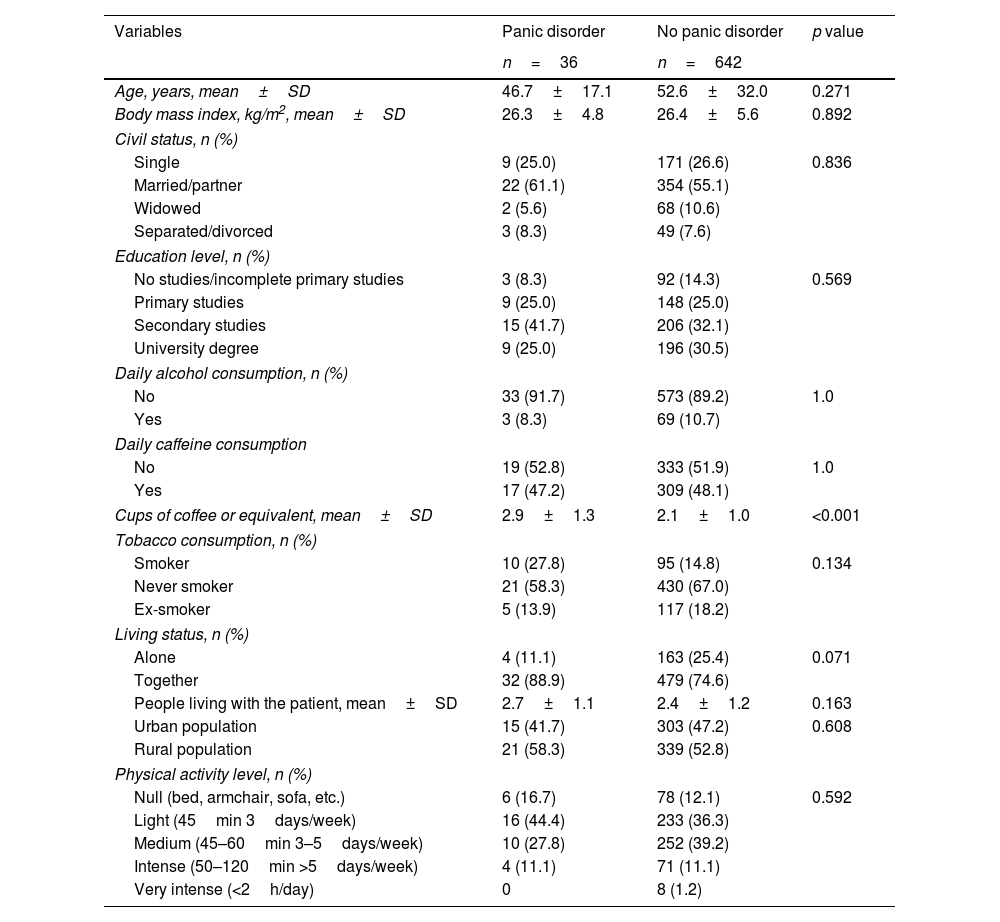
The comparison of sociodemographic characteristics between the groups of patients with and without panic disorder did not show statistically significant differences except for a higher amount of daily caffeine consumption among patients with panic disorder. (Table 1).
Sociodemographic data in the groups of patients with and without panic disorder.
| Variables | Panic disorder | No panic disorder | p value |
|---|---|---|---|
| n=36 | n=642 | ||
| Age, years, mean±SD | 46.7±17.1 | 52.6±32.0 | 0.271 |
| Body mass index, kg/m2, mean±SD | 26.3±4.8 | 26.4±5.6 | 0.892 |
| Civil status, n (%) | |||
| Single | 9 (25.0) | 171 (26.6) | 0.836 |
| Married/partner | 22 (61.1) | 354 (55.1) | |
| Widowed | 2 (5.6) | 68 (10.6) | |
| Separated/divorced | 3 (8.3) | 49 (7.6) | |
| Education level, n (%) | |||
| No studies/incomplete primary studies | 3 (8.3) | 92 (14.3) | 0.569 |
| Primary studies | 9 (25.0) | 148 (25.0) | |
| Secondary studies | 15 (41.7) | 206 (32.1) | |
| University degree | 9 (25.0) | 196 (30.5) | |
| Daily alcohol consumption, n (%) | |||
| No | 33 (91.7) | 573 (89.2) | 1.0 |
| Yes | 3 (8.3) | 69 (10.7) | |
| Daily caffeine consumption | |||
| No | 19 (52.8) | 333 (51.9) | 1.0 |
| Yes | 17 (47.2) | 309 (48.1) | |
| Cups of coffee or equivalent, mean±SD | 2.9±1.3 | 2.1±1.0 | <0.001 |
| Tobacco consumption, n (%) | |||
| Smoker | 10 (27.8) | 95 (14.8) | 0.134 |
| Never smoker | 21 (58.3) | 430 (67.0) | |
| Ex-smoker | 5 (13.9) | 117 (18.2) | |
| Living status, n (%) | |||
| Alone | 4 (11.1) | 163 (25.4) | 0.071 |
| Together | 32 (88.9) | 479 (74.6) | |
| People living with the patient, mean±SD | 2.7±1.1 | 2.4±1.2 | 0.163 |
| Urban population | 15 (41.7) | 303 (47.2) | 0.608 |
| Rural population | 21 (58.3) | 339 (52.8) | |
| Physical activity level, n (%) | |||
| Null (bed, armchair, sofa, etc.) | 6 (16.7) | 78 (12.1) | 0.592 |
| Light (45min 3days/week) | 16 (44.4) | 233 (36.3) | |
| Medium (45–60min 3–5days/week) | 10 (27.8) | 252 (39.2) | |
| Intense (50–120min >5days/week) | 4 (11.1) | 71 (11.1) | |
| Very intense (<2h/day) | 0 | 8 (1.2) | |
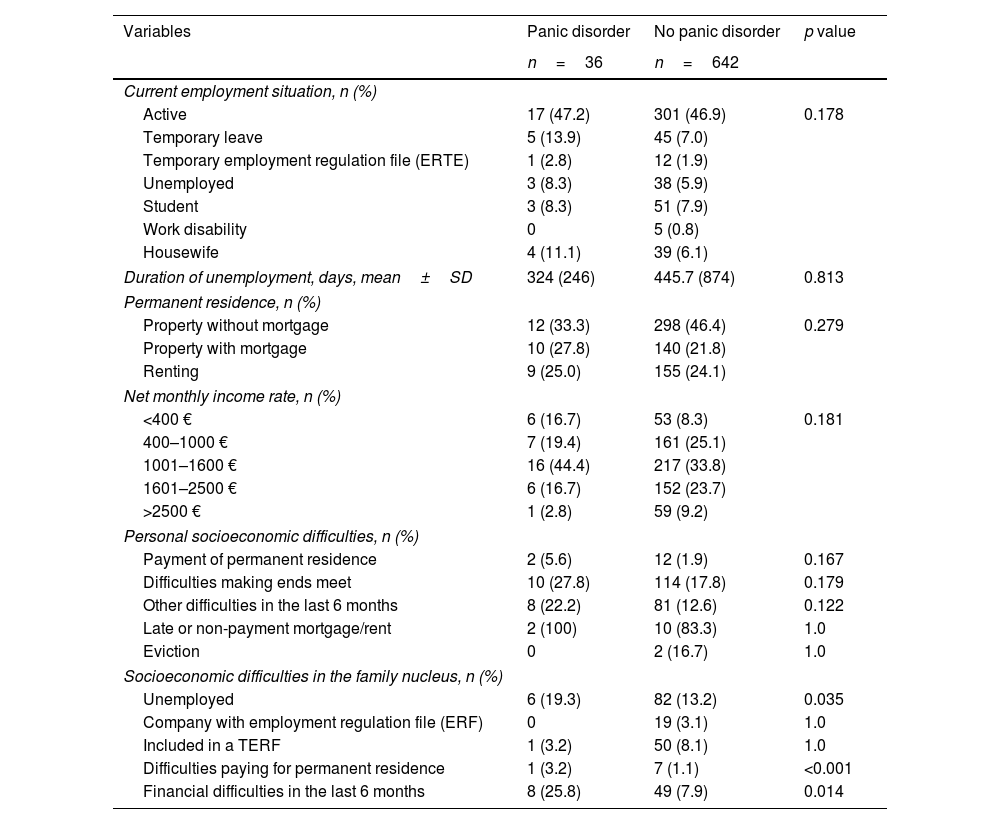
Results of socioeconomic findings are shown in Table 2. In general, almost half of the patients were employed, around 95% of them working in companies without employment regulations. Only 7 patients reported having a sick leave because of depression, with a median duration of 89 days. In around 95% of patients, the companies where the patients worked were not under an employment regulation file. The rate of unemployed patients was 8.3% and 5.9% in the groups of patients with and without panic disorder, with a median duration of being unemployed of 210 days. Regarding the characteristics of the patients’ permanent residence, property with mortgage and renting were the most frequent conditions (49.4% of the cases). The most common net monthly income rate was in the range between 1000€ and 1600€ (39% of the cases). Although more patients with panic disorder recognized having difficulties making ends meet and other personal socioeconomic problems in the last 6 months than those without panic disorder, differences were not significant. However, socioeconomic difficulties in the family (unemployed members, difficulties for paying permanent residence or financial problems in the last 6 months) were significantly more frequent among patients in the panic disorder group (Table 2).
Socioeconomic data in the groups of patients with and without panic disorder.
| Variables | Panic disorder | No panic disorder | p value |
|---|---|---|---|
| n=36 | n=642 | ||
| Current employment situation, n (%) | |||
| Active | 17 (47.2) | 301 (46.9) | 0.178 |
| Temporary leave | 5 (13.9) | 45 (7.0) | |
| Temporary employment regulation file (ERTE) | 1 (2.8) | 12 (1.9) | |
| Unemployed | 3 (8.3) | 38 (5.9) | |
| Student | 3 (8.3) | 51 (7.9) | |
| Work disability | 0 | 5 (0.8) | |
| Housewife | 4 (11.1) | 39 (6.1) | |
| Duration of unemployment, days, mean±SD | 324 (246) | 445.7 (874) | 0.813 |
| Permanent residence, n (%) | |||
| Property without mortgage | 12 (33.3) | 298 (46.4) | 0.279 |
| Property with mortgage | 10 (27.8) | 140 (21.8) | |
| Renting | 9 (25.0) | 155 (24.1) | |
| Net monthly income rate, n (%) | |||
| <400 € | 6 (16.7) | 53 (8.3) | 0.181 |
| 400–1000 € | 7 (19.4) | 161 (25.1) | |
| 1001–1600 € | 16 (44.4) | 217 (33.8) | |
| 1601–2500 € | 6 (16.7) | 152 (23.7) | |
| >2500 € | 1 (2.8) | 59 (9.2) | |
| Personal socioeconomic difficulties, n (%) | |||
| Payment of permanent residence | 2 (5.6) | 12 (1.9) | 0.167 |
| Difficulties making ends meet | 10 (27.8) | 114 (17.8) | 0.179 |
| Other difficulties in the last 6 months | 8 (22.2) | 81 (12.6) | 0.122 |
| Late or non-payment mortgage/rent | 2 (100) | 10 (83.3) | 1.0 |
| Eviction | 0 | 2 (16.7) | 1.0 |
| Socioeconomic difficulties in the family nucleus, n (%) | |||
| Unemployed | 6 (19.3) | 82 (13.2) | 0.035 |
| Company with employment regulation file (ERF) | 0 | 19 (3.1) | 1.0 |
| Included in a TERF | 1 (3.2) | 50 (8.1) | 1.0 |
| Difficulties paying for permanent residence | 1 (3.2) | 7 (1.1) | <0.001 |
| Financial difficulties in the last 6 months | 8 (25.8) | 49 (7.9) | 0.014 |
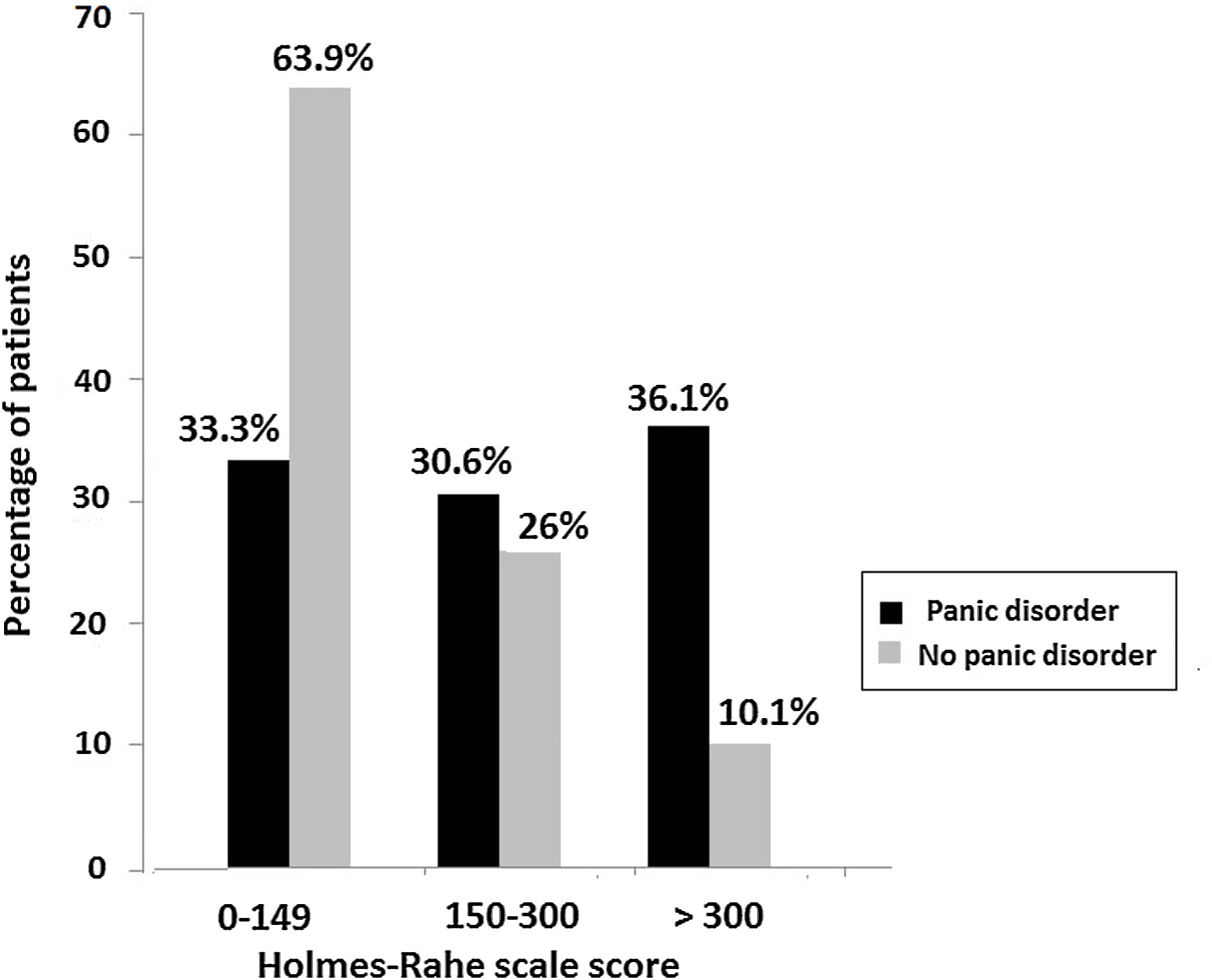
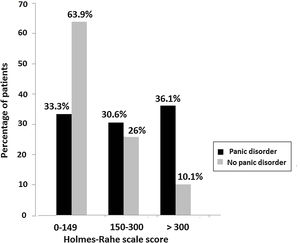
The total mean score of the Holmes–Rahe scale was 255.9±163.7 in patients with panic disorder and 136.8±134.7 in patients without panic disorder (p<0.001). As shown in Fig. 2, a higher number of patients with panic disorders had a high (score>300) and moderate (score 150–300) level of stress as compared with patients without panic disorder. A low level of stress (score<149) was significantly more frequent in patients without panic disorders.
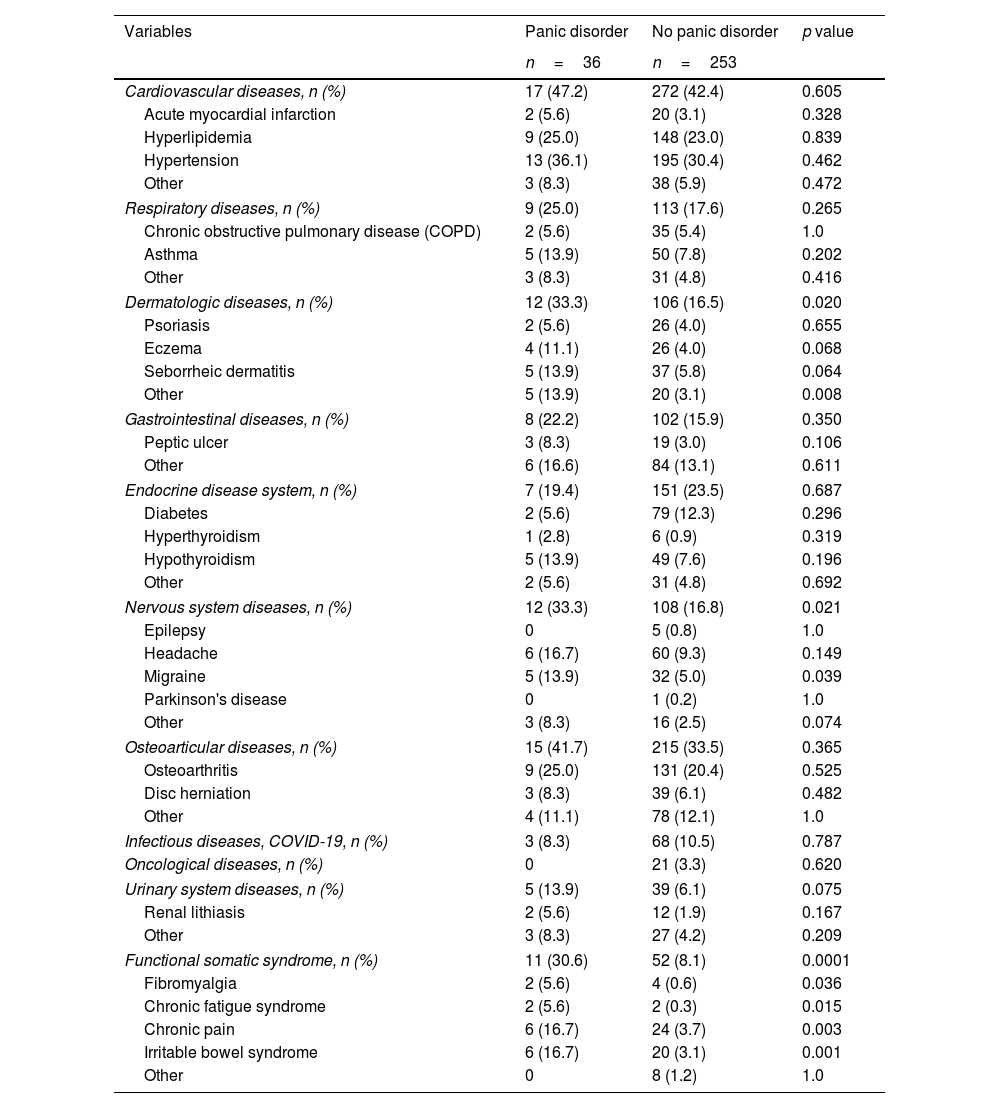
Patients with panic disorder showed more comorbidity than those without panic disorder, with statistically significant differences in dermatologic diseases, nervous system diseases, and functional somatic syndrome (Table 3). All pathological conditions included in the functional somatic syndrome, such as fibromyalgia, chronic fatigue syndrome, chronic pain, and irritable bowel syndrome were significantly more frequent among patients with panic disorder.
Comorbid diseases in the groups of patients with and without panic disorder.
| Variables | Panic disorder | No panic disorder | p value |
|---|---|---|---|
| n=36 | n=253 | ||
| Cardiovascular diseases, n (%) | 17 (47.2) | 272 (42.4) | 0.605 |
| Acute myocardial infarction | 2 (5.6) | 20 (3.1) | 0.328 |
| Hyperlipidemia | 9 (25.0) | 148 (23.0) | 0.839 |
| Hypertension | 13 (36.1) | 195 (30.4) | 0.462 |
| Other | 3 (8.3) | 38 (5.9) | 0.472 |
| Respiratory diseases, n (%) | 9 (25.0) | 113 (17.6) | 0.265 |
| Chronic obstructive pulmonary disease (COPD) | 2 (5.6) | 35 (5.4) | 1.0 |
| Asthma | 5 (13.9) | 50 (7.8) | 0.202 |
| Other | 3 (8.3) | 31 (4.8) | 0.416 |
| Dermatologic diseases, n (%) | 12 (33.3) | 106 (16.5) | 0.020 |
| Psoriasis | 2 (5.6) | 26 (4.0) | 0.655 |
| Eczema | 4 (11.1) | 26 (4.0) | 0.068 |
| Seborrheic dermatitis | 5 (13.9) | 37 (5.8) | 0.064 |
| Other | 5 (13.9) | 20 (3.1) | 0.008 |
| Gastrointestinal diseases, n (%) | 8 (22.2) | 102 (15.9) | 0.350 |
| Peptic ulcer | 3 (8.3) | 19 (3.0) | 0.106 |
| Other | 6 (16.6) | 84 (13.1) | 0.611 |
| Endocrine disease system, n (%) | 7 (19.4) | 151 (23.5) | 0.687 |
| Diabetes | 2 (5.6) | 79 (12.3) | 0.296 |
| Hyperthyroidism | 1 (2.8) | 6 (0.9) | 0.319 |
| Hypothyroidism | 5 (13.9) | 49 (7.6) | 0.196 |
| Other | 2 (5.6) | 31 (4.8) | 0.692 |
| Nervous system diseases, n (%) | 12 (33.3) | 108 (16.8) | 0.021 |
| Epilepsy | 0 | 5 (0.8) | 1.0 |
| Headache | 6 (16.7) | 60 (9.3) | 0.149 |
| Migraine | 5 (13.9) | 32 (5.0) | 0.039 |
| Parkinson's disease | 0 | 1 (0.2) | 1.0 |
| Other | 3 (8.3) | 16 (2.5) | 0.074 |
| Osteoarticular diseases, n (%) | 15 (41.7) | 215 (33.5) | 0.365 |
| Osteoarthritis | 9 (25.0) | 131 (20.4) | 0.525 |
| Disc herniation | 3 (8.3) | 39 (6.1) | 0.482 |
| Other | 4 (11.1) | 78 (12.1) | 1.0 |
| Infectious diseases, COVID-19, n (%) | 3 (8.3) | 68 (10.5) | 0.787 |
| Oncological diseases, n (%) | 0 | 21 (3.3) | 0.620 |
| Urinary system diseases, n (%) | 5 (13.9) | 39 (6.1) | 0.075 |
| Renal lithiasis | 2 (5.6) | 12 (1.9) | 0.167 |
| Other | 3 (8.3) | 27 (4.2) | 0.209 |
| Functional somatic syndrome, n (%) | 11 (30.6) | 52 (8.1) | 0.0001 |
| Fibromyalgia | 2 (5.6) | 4 (0.6) | 0.036 |
| Chronic fatigue syndrome | 2 (5.6) | 2 (0.3) | 0.015 |
| Chronic pain | 6 (16.7) | 24 (3.7) | 0.003 |
| Irritable bowel syndrome | 6 (16.7) | 20 (3.1) | 0.001 |
| Other | 0 | 8 (1.2) | 1.0 |
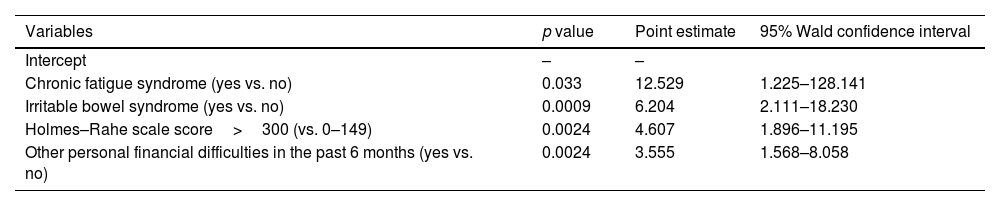
In the multivariate analysis, chronic fatigue syndrome, other personal socioeconomic difficulties in the last 6 months, irritable bowel syndrome, and a score>300 in the Holmes–Rahe scale were independent variables significantly associated with panic disorder (Table 4).
Analysis of maximum likelihood estimates: variables associated with panic disorder.
| Variables | p value | Point estimate | 95% Wald confidence interval |
|---|---|---|---|
| Intercept | – | – | |
| Chronic fatigue syndrome (yes vs. no) | 0.033 | 12.529 | 1.225–128.141 |
| Irritable bowel syndrome (yes vs. no) | 0.0009 | 6.204 | 2.111–18.230 |
| Holmes–Rahe scale score>300 (vs. 0–149) | 0.0024 | 4.607 | 1.896–11.195 |
| Other personal financial difficulties in the past 6 months (yes vs. no) | 0.0024 | 3.555 | 1.568–8.058 |
In this study the prevalence of panic disorder was 5.3%, which is lower than prevalence rates of 9.7% and 15.7% reported in two previous similar studies for the years 2006 and 2010, respectively.13,14 In both studies, however, in which the same PRIME-MD instrument was used, the number of surveyed patients was much larger (7929 and 5876 patients, respectively). Also, one of these studies14 was carried out during the economic crisis that began in 2007 and it was found that recession had significantly increased the frequency of mental health disorders among primary care attendees in Spain, particularly among families experiencing unemployment and mortgage payment difficulties. In the present survey and although the interviews were face-to-face, the restrictions imposed by the second and third waves in Spain may explain the lower number of primary care physicians who agreed to participate in the study. However, other studies conducted in the primary care setting showed percentages of patients with panic disorders like the present results. In a study of 15 US primary care clinics, Generalized Anxiety Disorder (GAD)-7 scale was administered to a random sample of 965 patients, with a rate of panic disorder of 6.8% (95% CI 5.3–8.6%).19
In a cross-sectional study with patients from three primary care centers in Brazil using the Mini International Neuropsychiatric Interview (MINI) to diagnose panic disorder, the prevalence of panic disorder was 5.6% among 1081 patients evaluated.20
Panic disorder was more frequently diagnosed in women (64% of the cases). Women have consistently higher prevalence rates of anxiety disorders, which are also more disabling than in man.21 In agreement with data reported in the literature,22–24 medical illnesses were more frequent among patients with panic disorders, in particular fibromyalgia, chronic pain, chronic fatigue syndrome and irritable bowel syndrome. Pain and other functional somatic symptoms may be the primary complaints in patients with anxiety disorders seen in primary care.25–27 Chronic fatigue syndrome and irritable bowel disease were significant factors independently associated with panic disorder in our study population. The comorbidity between irritable bowel syndrome and anxiety disorders is high, and anxiety and depression may contribute to inefficient therapies of gastrointestinal complaints in these patients.28,29
In the analysis of the impact of stressful events during COVID-19 pandemic, there was a clear association between scores of the Holmes–Rahe scale and the presence of panic disorder. A score>300 indicating a high level of external stressor was a significant factor associated with panic disorder. About 30% of patients with panic disorder showed scores above 150 life change units, as an indicator for a major breakdown in mental health status according to the Holmes–Rahe stress load. However, among patients without panic disorder, the level of stress was moderate in 26% of cases and high in only 10%. The early stages of the COVID-19 pandemic were often associated with increased levels of distress, although longitudinal follow-up studies showed remarkable signs of resilience.30 However, there is a lack of evidence from studies carried out during the pandemics that can inform the selection of interventions that are beneficial to the resilience, which could therefore be used to support mental well-being.31
In relation to the effect socioeconomic difficulties triggered by COVID-19 pandemic, having personal financial difficulties in the past 6 months was a risk factor for panic disorder. Moreover, the percentages of unemployed (patients and members in the family nucleus), very low monthly income rate (<400 €), difficulties making ends meet, and late or non-payment mortgage/rent were higher in the group of panic disorder. Also, patients without panic disorders showed higher percentages in high monthly income rates (>2500 €) and having a property without mortgage, and lower percentages of financial difficulties in the family nucleus. In a previous study of the mental health risks of 2010 economic crisis in Spain as compared to the pre-crisis period of 2006, about one-third of the overall risk in the population with mental health disorders attended in primary care could be attributed to combined risks of household unemployment and mortgage payment difficulties.14
Limitations of the study include the reduced participation of primary care physicians, which affected the recruitment of patients, although the use of the PRIME-MD instrument for the diagnosis of panic disorder is a strength of the study. Other limitations may include memory bias or social desirability. The impact of COVID-19 pandemic on the mental health of healthcare workers in primary care was not evaluated in our study. However, in a multicenter, cross-sectional, web-based survey conducted in 2928 primary healthcare workers in Spain, between May and September 2020, a high proportion of participants (43.7%) had a current mental disorder, with a prevalence rate lower for males than for females, who also showed a greater risk of psychological distress related to greater occupational exposure to patients with COVID-19.32
ConclusionsIn this study of non-selected consecutive primary care attendees in real-world conditions during the second and three waves of the COVID-19 pandemic, the prevalence of panic disorder was 5.3%, being more frequent in women. A high level of stress, concomitant chronic fatigue syndrome and irritable bowel disease, and having financial difficulties in the past 6 months were significant factors associated with panic disorder during the COVID-19.
- •
The impact of COVID-19 on the mental sphere includes anxiety, depression, psychological distress, fear, loneliness, and sleep disturbance.
- •
In the socioeconomic area, concerns regarding employment and finances have been highlighted.
- •
There is little evidence of the prevalence of panic disorder during COVID-19 pandemic in patients attended in the primary healthcare.
- •
In a consecutive non-selected population of primary care patients visited during the second and third waves of COVID-19 pandemic, the prevalence of panic disorder was 5.3%.
- •
The diagnosis was established using a validated version of the Primary Care Evaluation Mental Disorders (PRIME-MD).
- •
High level of stress, concomitant chronic fatigue syndrome, irritable bowel disease, and having financial difficulties in the past 6 months were independent predictive factors of panic disorder.
Conceptualization, M.G.P. and M.R.B.; methodology, M.G.P., M.R.B., A.T.V. and V.G.M.; validation, M.G.P. and M.R.B.; formal analysis, M.G.P. and M.R.B; investigation, A.T.V. and V.G.M.; writing—original draft preparation, M.G.P. and M.R.B.; writing—review and editing, M.G.P., M.R.B., A.T.V. and V.G.M. All authors have read and agreed to the published version of the manuscript.
Ethical considerationsThe study was approved by the Clinical Research Ethics Committee (CEIC) of Hospital Clínico San Carlos (code 20/701E, 2020). Informed consent was obtained from all subjects involved in the study.
FundingThe study was supported by a Pfizer Competitive Global Grant (ID: 63317657).
Conflicts of interestMiquel Roca received research funding from Janssen, Lundbeck and Pfizer. The other authors declare that they have no conflicts of interest.
The authors thank Grupo SANED, S.L., for logistic support and Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.