Abstract
Introduction
Aim of this analysis was to report toxicity and clinical outcomes in oligorecurrent prostate cancer (PCa) patients treated with single fraction stereotactic radiosurgery (SRS) for bone metastases.
Methods
We separately analyzed clinical data of PCa patients with bone oligometastases enrolled in a prospective phase I trial (DESTROY-2). DESTROY-2 was based on SRS delivered using volumetric modulated arc therapy in patients with primary or metastatic tumors in several extra-cranial body sites. Acute and late toxicity, biochemical tumor response, local control (LC), distant metastases-free (DPFS), progression-free (PFS), time to next-line systemic treatment-free (NEST-FS), and overall survival (OS) were calculated.
Results
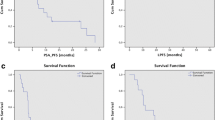
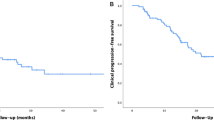
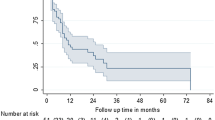
Data on 37 PCa patients, carrying out 50 bone metastases, candidates for curative-intent treatment and treated with SRS at our Institution were collected. SRS dose ranged between 12 and 24 Gy. One grade 1 acute skin toxicity in one patient treated on the hip (24 Gy) and one grade 1 late skin toxicity in a patient with a scapular lesion (24 Gy) were recorded. No cases of bone fracture were registered in the treated population. With a median follow-up of 25 months (range 3–72 months) 2-year actuarial LC, DPFS, PFS, and OS were 96.7%, 58.1%, 58.1%, and 95.8%, respectively. Median and 2-year NEST-FS were 30 months (range 1–69 months) and 51.2%, respectively.
Conclusions
Data analysis showed few toxicity events, high local control rate and prolonged NEST-FS after linear accelerator-based radiosurgery of bone oligometastases from PCa. The possibility of postponing systemic treatments in patients with oligometastatic PCa by means of SRS should be taken into account. Further prospective studies on larger series are needed to confirm the reported results.

Similar content being viewed by others
Data availability
Data will be made available on reasonable request.
Abbreviations
- PCa:
-
Prostate cancer
- PSMA-PET:
-
Prostate-specific membrane antigen positron emission tomography
- SBRT:
-
Stereotactic body radiotherapy
- SRS:
-
Stereotactic radiosurgery
- LC:
-
Local control
- VMAT:
-
Volumetric modulated Arc therapy
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- PTV:
-
Planning target volume
- ECOG-PS:
-
Eastern cooperative oncology group performance status
- PSA:
-
Prostate serum antigen
- NEST-FS:
-
Time to next-line systemic treatment-free survival
- DPFS:
-
Distant progression-free survival
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- VAS:
-
Pain visual analog scale
- BED:
-
Biological equivalent dose
References
Mazzone E, Preisser F, Nazzani S, et al. Location of metastases in contemporary prostate cancer patients affects cancer-specific mortality. Clin Genitourin Cancer. 2018;16:376-384.e1.
Gandaglia G, Karakiewicz PI, Briganti A, et al. Impact of the site of metastases on survival in patients with metastatic prostate cancer. Eur Urol. 2015;68(2):325–34.
Corfield J, Perera M, Bolton D, et al. (68) Ga-prostate specific membrane antigen (PSMA) positron emission tomography (PET) for primary staging of high-risk prostate cancer: a systematic review. World J Urol. 2018;36:519–27.
Hofman MS, Lawrentschuk N, Francis RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet. 2020;395:1208–16.
Perera M, Papa N, Roberts M, et al. Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: a systematic review and meta-analysis. Eur Urol. 2020;77:403–17.
Zhou J, Gou Z, Wu R, et al. Comparison of PSMA-PET/CT, choline-PET/CT, NaF-PET/CT, MRI, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate cancer: a systematic review and meta-analysis. Skeletal Radiol. 2019;48:1915–24.
Phillips R, Shi WY, Deek M, et al. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 2020;6(5):650–9.
Guckenberger M, Lievens Y, Bouma AB, et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020;21(1):e18–28.
Berkovic P, De Meerleer G, Bieke L, et al. Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: deferring androgen deprivation therapy. Clin Genitourin Cancer. 2013;11:27–32.
Decaestecker K, De Meerleer G, Ameye F, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence (STOMP): study protocol for a randomized phase II trial. BMC Cancer. 2014;14:671.
Ingrosso G, Trippa F, Maranzano E, et al. Stereotactic body radiotherapy in oligometastatic prostate cancer patients with isolated lymph nodes involvement: a two-institution experience. World J Urol. 2017;35(1):45–9.
Deodato F, Macchia G, Grimaldi L, et al. Stereotactic radiotherapy in recurrent gynecological cancer: a case series. Oncol Rep. 2021;22:415–9.
Macchia G, Morganti AG, Cilla S, et al. Quality of life and toxicity of stereotactic radiotherapy in pancreatic tumors: a case series. Cancer Invest. 2012;30:149–55.
Deodato F, Cilla S, Macchia G, et al. Extracranial radiosurgery with volumetric modulated arc therapy: Feasibility evaluation of a phase I trial. Oncol Lett. 2013;5:1889–96.
Macchia G, Deodato F, Cilla S, et al. Volumetric intensity modulated arc therapy for stereotactic body radiosurgery in oligometastatic breast and gynecological cancers: feasibility and clinical results. Oncol Rep. 2014;32(5):2237–43.
Deodato F, Cilla S, Macchia G, et al. Stereotactic radiosurgery (SRS) with volumetric modulated arc therapy (VMAT): interim results of a multi-arm phase I trial (DESTROY-2). Clin Oncol (R Coll Radiol). 2014;26(12):748–56.
National Cancer Institute (2020) Common terminology criteria for adverse events v.4.03 (CTCAE v.4.03). https://ctep.cancer.gov/protocolDevelopment
Cornford P, Bellmunt J, Bolla M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol. 2017;71:630–42.
Hurkmans CW, Cuijpers JP, Lagerwaard FJ, et al. Recommendations for implementing stereotactic radiotherapy in peripheral stage IA non-small cell lung cancer: report from the Quality Assurance Working Party of the randomised phase III ROSEL study. Radiat Oncol. 2009;4:1.
Jereczek-Fossa BA, Fanetti G, Fodor C, et al. Salvage stereotactic body radiotherapy for isolated lymph node recurrent prostate cancer: single institution series of 94 consecutive patients and 124 lymph nodes. Clin Genitourin Cancer. 2017;15(4):e623–32.
Jereczek-Fossa BA, Beltramo G, Fariselli L, et al. Robotic image-guided stereotactic radiotherapy, for isolated recurrent primary, lymph node or metastatic prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82(2):889–97.
Viani GA, Arruda CV, Hamamura AC, et al. Stereotactic body radiotherapy for oligometastatic prostate cancer recurrence: a meta-analysis. Am J Clin Oncol. 2020. https://doi.org/10.1097/COC.0000000000000635.
Napieralska A, Miszczyk L, Stapor-Fudzinska M, et al. CyberKnife stereotactic radiosurgery and stereotactic ablative radiation therapy of patients with prostate cancer bone metastases. Neoplasma. 2016;63(2):304–12.
Napieralska A, Miszczyk L, Tukiendorf A, Stąpór-Fudzińska M, et al. The results of treatment of prostate cancer bone metastases after CyberKnife radiosurgery. Ortop Traumatol Rehabil. 2014;16(3):339–49.
Muacevic A, Kufeld M, Rist C, et al. Safety and feasibility of image-guided robotic radiosurgery for patients with limited bone metastases of prostate cancer. Urol Oncol. 2013;31(4):455–60.
Spencer KL, van der Velden JM, Wong E, et al. Systematic review of the role of stereotactic radiotherapy for bone metastases. J Natl Cancer Inst. 2019;111(10):1023–32.
Siva S, Bressel M, Murphy DG, et al. Stereotactic ablative body radiotherapy (SABR) for oligometastatic prostate cancer: a prospective clinical trial. Eur Urol. 2018;74(4):455–62.
Erler D, Brotherston D, Sahgal A, et al. Local control and fracture risk following stereotactic body radiation therapy for non-spine bone metastases. Radiother Oncol. 2018;127(2):304–9.
Cunha MV, Al-Omair A, Atenafu EG, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012;84(3):e343–9.
Berkovic P, De Meerleer G, Delrue L, et al. Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: deferring androgen deprivation therapy. Clin Genitourin Cancer. 2013;11(1):27–32.
Ost P, Jereczek-Fossa BA, As NV, Zilli T, et al. Progression-free survival following stereotactic body radiotherapy for oligometastatic prostate cancer treatment-naive recurrence: a multi-institutional analysis. Eur Urol. 2016;69(1):9–12.
Triggiani L, Mazzola R, Maria S, et al. Metastasis-directed stereotactic radiotherapy for oligoprogressive castration-resistant prostate cancer: a multicenter study. World J Urol. 2019;37:2631–7.
Hurmuz P, Onal C, Ozyigit G et al. Treatment outcomes of metastasis-directed treatment using (68)Ga-PSMA-PET/CT for oligometastatic or oligorecurrent prostate cancer: Turkish Society for Radiation Oncology group study (TROD 09–002) Strahlentherapie und Onkologie: Organ der Deutschen Rontgengesellschaft.
Schick U, Jorcano S, Nouet P, et al. Androgen deprivation and high-dose radiotherapy for oligometastatic prostate cancer patients with less than five regional and/or distant metastases. Acta Oncol. 2013;52(8):1622–8.
Rogowski P, Roach M 3rd, Schmidt-Hegemann NS, et al. Radiotherapy of oligometastatic prostate cancer: a systematic review. Radiat Oncol. 2021;16(1):50. https://doi.org/10.1186/s13014-021-01776-8.PMID:33750437;PMCID:PMC7941976.
Triggiani L, Alongi F, Buglione M, et al. Efficacy of stereotactic body radiotherapy in oligorecurrent and in oligoprogressive prostate cancer: new evidence from a multicentric study. Br J Cancer. 2017;116(12):1520–5.
Habl G, Straube C, Schiller K, et al. Oligometastases from prostate cancer: local treatment with stereotactic body radiotherapy (SBRT). BMC Cancer. 2017;17(1):361.
Tucci M, Leone G, Buttigliero C, et al. Hormonal treatment and quality of life of prostate cancer patients: new evidence. Minerva Urol Nefrol. 2018;70(2):144–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical approval
The trial was approved by the local Institutional Review Board (P#988/CE/2010).
Informed consent
All the patients gave their informed consent prior to their inclusions in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deodato, F., Pezzulla, D., Cilla, S. et al. Stereotactic radiosurgery for bone metastases in oligometastatic prostate cancer patients: DESTROY-2 clinical trial subanalysis. Clin Transl Oncol 24, 1177–1183 (2022). https://doi.org/10.1007/s12094-021-02764-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02764-w