Abstract
Introduction
Papillary thyroid cancer (PTC) is the predominant histological type of thyroid cancer, accounting for 80% of thyroid cancers. MiR-181a is a novel microRNA that is usually upregulated in multiple cancers. This study aims to explore the role and underlying mechanism of miR-181a in PTC.
Methods
CCK8 and Transwell assays were performed to evaluate cell viability and migration. The mRNA level of miR-181a and KLF15 was calculated by qRT-PCR. The protein level of E-Cadherin, N-Cadherin and GAPDH was evaluated by western blot. Dual luciferase assay was conducted to validate that miR-181a directly targeting the 3′-UTR of KLF15 mRNA in TPC-1 cells.
Results
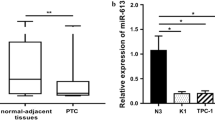
We observed that miR-181a was overexpressed and KLF15 was low expressed in PTC tissues and cell lines. Upregulation of miR-181a or downregulation of KLF15 predicted poor outcomes in PTC patients. MiR-181a improved cell growth of PTC, migration and epithelial–mesenchymal transition (EMT) in TPC-1 cells. KLF15 was a target gene of miR-181a and its expression was mediated by miR-181a. KLF15 partially reversed the facilitating effect of miR-181a on cell proliferation and migration in TPC-1 cells.
Conclusion
We discovered that miR-181a served as an oncogene downregulating KLF15, thereby inhibiting cell proliferation, migration and the EMT. These findings demonstrate that miR-181a plays a significant role in PTC progression and could be a therapeutic target for PTC.






Similar content being viewed by others

References
Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet. 2016;388(10061):2783–95. https://doi.org/10.1016/S0140-6736(16)30172-6.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. https://doi.org/10.3322/caac.21442.
Pelizzo MR, Merante BI, Toniato A, et al. Diagnosis, treatment, prognostic factors and long-term outcome in papillary thyroid carcinoma. Minerva Endocrinol. 2008;33(4):359–79.
La Vecchia C, Malvezzi M, Bosetti C, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015;136(9):2187–95. https://doi.org/10.1002/ijc.29251.
Schneider DF, Chen H. New developments in the diagnosis and treatment of thyroid cancer. CA Cancer J Clin. 2013;63(6):374–94. https://doi.org/10.3322/caac.21195.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–33. https://doi.org/10.1016/j.cell.2009.01.002.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97. https://doi.org/10.1016/s0092-8674(04)00045-5.
Liu H, Chen X, Lin T, Chen X, Yan J, Jiang S. MicroRNA-524-5p suppresses the progression of papillary thyroid carcinoma cells via targeting on FOXE1 and ITGA3 in cell autophagy and cycling pathways. J Cell Physiol. 2019;234(10):18382–91. https://doi.org/10.1002/jcp.28472.
Liu F, Yin R, Chen X, et al. Over-expression of miR-206 decreases the Euthyrox-resistance by targeting MAP4K3 in papillary thyroid carcinoma. Biomed Pharmacother. 2019;114: 108605. https://doi.org/10.1016/j.biopha.2019.108605.
Wang D, Guo C, Kong T, Mi G, Li J, Sun Y. Serum miR-22 may be a biomarker for papillary thyroid cancer. Oncol Lett. 2019;17(3):3355–61. https://doi.org/10.3892/ol.2019.10011.
Ortiz I, Barros-Filho MC, Dos RM, et al. Loss of DNA methylation is related to increased expression of miR-21 and miR-146b in papillary thyroid carcinoma. Clin Epigenetics. 2018;10(1):144. https://doi.org/10.1186/s13148-018-0579-8.
Wei F, Yang S, Wang S. MicroRNAs: a critical regulator under mechanical force. Histol Histopathol. 2018;33(4):335–42. https://doi.org/10.14670/HH-11-924.
Sun W, Wang X, Li J, et al. MicroRNA-181a promotes angiogenesis in colorectal cancer by targeting SRCIN1 to promote the SRC/VEGF signaling pathway. Cell Death Dis. 2018;9(4):438. https://doi.org/10.1038/s41419-018-0490-4.
Kozloski GA, Jiang X, Bhatt S, et al. miR-181a negatively regulates NF-kappaB signaling and affects activated B-cell-like diffuse large B-cell lymphoma pathogenesis. Blood. 2016;127(23):2856–66. https://doi.org/10.1182/blood-2015-11-680462.
Yuan R, Liu N, Yang J, Peng J, Liu L, Guo X. The expression and role of miR-181a in multiple myeloma. Medicine (Baltimore). 2018;97(35): e12081. https://doi.org/10.1097/MD.0000000000012081.
Yu J, Qi J, Sun X, et al. MicroRNA181a promotes cell proliferation and inhibits apoptosis in gastric cancer by targeting RASSF1A. Oncol Rep. 2018;40(4):1959–70. https://doi.org/10.3892/or.2018.6632.
Li Y, Kuscu C, Banach A, et al. miR-181a-5p inhibits cancer cell migration and angiogenesis via downregulation of matrix metalloproteinase-14. Cancer Res. 2015;75(13):2674–85. https://doi.org/10.1158/0008-5472.CAN-14-2875.
Uchida S, Tanaka Y, Ito H, et al. Transcriptional regulation of the CLC-K1 promoter by myc-associated zinc finger protein and kidney-enriched Kruppel-like factor, a novel zinc finger repressor. Mol Cell Biol. 2000;20(19):7319–31. https://doi.org/10.1128/mcb.20.19.7319-7331.2000.
Zhao Y, Cai L. Does Kruppel like factor 15 play an important role in the left ventricular hypertrophy of patients with type 2 diabetes? EBioMedicine. 2017;20:17–8. https://doi.org/10.1016/j.ebiom.2017.05.009.
Pearson R, Fleetwood J, Eaton S, Crossley M, Bao S. Kruppel-like transcription factors: a functional family. Int J Biochem Cell Biol. 2008;40(10):1996–2001. https://doi.org/10.1016/j.biocel.2007.07.018.
Zhou J, Tan T, Tian Y, et al. Kruppel-like factor 15 activates hepatitis B virus gene expression and replication. Hepatology. 2011;54(1):109–21. https://doi.org/10.1002/hep.24362.
Ray S, Pollard JW. KLF15 negatively regulates estrogen-induced epithelial cell proliferation by inhibition of DNA replication licensing. Proc Natl Acad Sci USA. 2012;109(21):E1334–43. https://doi.org/10.1073/pnas.1118515109.
Yoda T, McNamara KM, Miki Y, et al. KLF15 in breast cancer: a novel tumor suppressor? Cell Oncol (Dordr). 2015;38(3):227–35. https://doi.org/10.1007/s13402-015-0226-8.
Gao L, Qiu H, Liu J, et al. KLF15 promotes the proliferation and metastasis of lung adenocarcinoma cells and has potential as a cancer prognostic marker. Oncotarget. 2017;8(66):109952–61. https://doi.org/10.18632/oncotarget.21972.
Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017;317(13):1338–48. https://doi.org/10.1001/jama.2017.2719.
Kim SJ, Myong JP, Jee HG, et al. Combined effect of Hashimoto’s thyroiditis and BRAF(V600E) mutation status on aggressiveness in papillary thyroid cancer. Head Neck. 2016;38(1):95–101. https://doi.org/10.1002/hed.23854.
Lee YS, Dutta A. MicroRNAs in cancer. Annu Rev Pathol. 2009;4:199–227. https://doi.org/10.1146/annurev.pathol.4.110807.092222.
Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6(11):857–66. https://doi.org/10.1038/nrc1997.
Ji D, Chen Z, Li M, et al. MicroRNA-181a promotes tumor growth and liver metastasis in colorectal cancer by targeting the tumor suppressor WIF-1. Mol Cancer. 2014;13:86. https://doi.org/10.1186/1476-4598-13-86.
Ge S, Zhang H, Deng T, et al. MiR-181a, a new regulator of TGF-beta signaling, can promote cell migration and proliferation in gastric cancer. Invest New Drugs. 2019. https://doi.org/10.1007/s10637-018-0695-5.
Brabletz T, Kalluri R, Nieto MA, Weinberg RA. EMT in cancer. Nat Rev Cancer. 2018;18(2):128–34. https://doi.org/10.1038/nrc.2017.118.
Chaffer CL, San JB, Lim E, Weinberg RA. EMT, cell plasticity and metastasis. Cancer Metastasis Rev. 2016;35(4):645–54. https://doi.org/10.1007/s10555-016-9648-7.
Parikh A, Lee C, Joseph P, et al. microRNA-181a has a critical role in ovarian cancer progression through the regulation of the epithelial-mesenchymal transition. Nat Commun. 2014;5:2977. https://doi.org/10.1038/ncomms3977.
McConnell BB, Yang VW. Mammalian Kruppel-like factors in health and diseases. Physiol Rev. 2010;90(4):1337–81. https://doi.org/10.1152/physrev.00058.2009.
Kim YD, Hwang SL, Jeon HJ, et al. B-cell translocation gene 2 enhances fibroblast growth factor 21 production by inducing Kruppel-like factor 15. Sci Rep. 2019;9(1):3730. https://doi.org/10.1038/s41598-019-40359-2.
Wang X, He M, Li J, Wang H, Huang J. KLF15 suppresses cell growth and predicts prognosis in lung adenocarcinoma. Biomed Pharmacother. 2018;106:672–7. https://doi.org/10.1016/j.biopha.2018.07.006.
Sun C, Ma P, Wang Y, et al. KLF15 inhibits cell proliferation in gastric cancer cells via up-regulating CDKN1A/p21 and CDKN1C/p57 expression. Dig Dis Sci. 2017;62(6):1518–26. https://doi.org/10.1007/s10620-017-4558-2.
Yang L, Wei QM, Zhang XW, et al. MiR-376a promotion of proliferation and metastases in ovarian cancer: potential role as a biomarker. Life Sci. 2017;15(173):62–7. https://doi.org/10.1016/j.lfs.2016.12.007.
Wang K, Ren Y, Liu Y, et al. miR-4262 promotes proliferation and invasion of human breast cancer cells through directly targeting KLF6 and KLF15. Oncol Res. 2017;25(2):277–83. https://doi.org/10.3727/096504016X14732514133203.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in this work.
Ethical approval
The study was approved by the Ethics Committee of Yantaishan Hospital. The study was performed according to the Declaration of Helsinki.
Informed consent
All study actions were performed under the appropriate ethics code, and consent was obtained from all patients within the clinical trial recruited for treatment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, C.X., Liu, B.J., Su, Y. et al. MiR-181a promotes cell proliferation and migration through targeting KLF15 in papillary thyroid cancer. Clin Transl Oncol 24, 66–75 (2022). https://doi.org/10.1007/s12094-021-02670-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02670-1